Understanding Ambulance Costs
Link to Article: https://www.healthcare.com/blog/why-ambulances-expensive/
Here’s Why Ambulances Are So Expensive
Updated: April 25, 2019 Published: July 12, 2017
Image:ER24 EMS (Pty) Ltd. / Flickr
From the equipment costs and employee salaries to flaws in how EMS services are reimbursed, there are many factors that contribute to our high ambulance costs.
As we’ve covered before, emergency medical services (EMS) often cost more than you think. Ambulance bills can exceed $1,000 and occasionally even reach $2,000. We spoke with Scott Moore, the human resources and operational consultant at the American Ambulance Association to try to get to the bottom of why ambulances are so expensive.
Equipment and Workers Cost Money
When you receive a bill for an ambulance ride, rarely do you think about all the costs that go into the vehicle before you ever dial 9-1-1.
“People just don’t consider the costs that go into purchasing an ambulance,” says Moore. “For instance, my town just purchased a new ambulance. It was $225,000 for that vehicle. You can get ambulances cheaper than that but the average box-style ambulance costs between $125,000 to $150,000.”
It’s not just the vehicles either. Moore goes on to explain the loads of equipment and medication that need to be accounted for. Not only are these things already expensive, but they’re actually getting more costly.
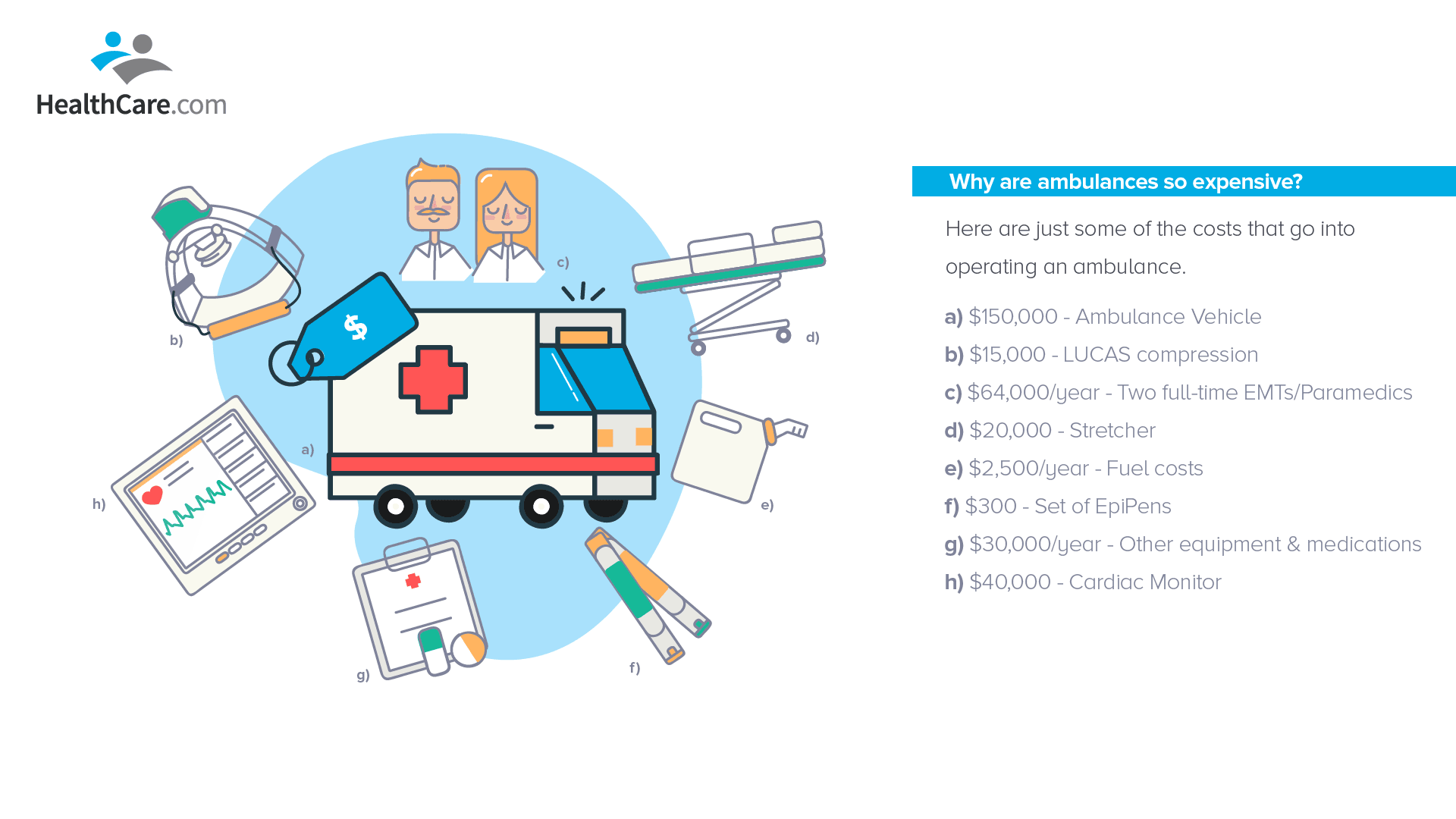 Stretchers, which were only $2,500 in the 1990s, can now cost as much as $40,000. Cardiac monitors also cost around $40,000. A LUCAS compression machine, which applies better compression than any human could possibly do, has a price tag of around $15,000. Then there are the copious amount of smaller costs, like $300 for a set of EpiPens, that add up; that includes the hundreds of medications that need to be continually restocked, gas costs, and vehicle maintenance.
Stretchers, which were only $2,500 in the 1990s, can now cost as much as $40,000. Cardiac monitors also cost around $40,000. A LUCAS compression machine, which applies better compression than any human could possibly do, has a price tag of around $15,000. Then there are the copious amount of smaller costs, like $300 for a set of EpiPens, that add up; that includes the hundreds of medications that need to be continually restocked, gas costs, and vehicle maintenance.
“Look, we can’t just say, ‘this patient needs epinephrine, lets run out and get some.’ We always need to be ready so those costs are there,” says Moore.
Aside from the equipment needs, there’s also staffing costs. According to Moore, when you need at least two field providers per ambulance working at any given time (covering all 24 hours of the day and all seven days of the week), the costs can be staggering. Including the insurance benefits provided to field workers, the average costs spent on EMS workers increase by 10 percent annually.
Medicare and Medicaid Underpay for Services
Actually getting paid for the services EMS provides is a sensitive issue, especially when it comes to reimbursements from government programs like Medicare and Medicaid.
“Reimbursements are the biggest issue facing EMS today,” Moore says. “If you look back at [Government Accountability Office] reports then you will see that they have been reimbursing at less than what it costs.”
Moore is right. A 2012 report from the Government Accountability Office (GAO) shows that average Medicare reimbursements rates for EMS are -1 percent. In other words, Medicare is paying slightly less for ambulance rides than the rides actually cost.
Medicaid pays even less, with rates as much as 40 percent lower than what Medicare pays.
As costs of EMS services continue to rise, Medicare and Medicaid rates have stagnated or even decreased.
“Reimbursement rates from Medicare and Medicaid have stayed the same or gone down every year for the past 20 years. It sounds crazy to me. It’s as if the government came in and said ‘you did some work for the federal government; we are going to pay you a little bit less than it costs to actually do the work, but that’s the way it works if you want to play in the game.’”
Insurance Companies Follow Suit
When the government underpays EMS providers, it has ripple effects – and it’s contributed greatly to why ambulances are so expensive. Insurance companies see those low reimbursement rates and cry foul when they are required to pay more.
Moore encountered this himself when he negotiated a contract with the largest insurance provider in his state.
“I tried to work with Blue Cross Blue Shield and when I was negotiating they said ‘that’s what Medicare pays. Why are you charging us more? You’re gouging us.’ And I said ‘Medicare is paying us less than it costs, you need to pay us more than that. We are entitled to cover costs.”
It is important to note that EMS industry leaders are not solely motivated by profit margins. They are just looking to cover costs. Most ambulance workers join the field for far nobler reasons than for the money they will earn, which isn’t much. Moore actually took a pay cut when he left his job at a local grocery store to start working in EMS.
If insurance companies start paying more for EMS services, he believes they will see innumerable long-term savings.
Let’s say you need a cath lab and you decide not to take an ambulance because it’s too costly. You’ll get to the emergency room and be forced to wait for hours, all the while your heart fails. That wait time can require you to pay for costly maintenance heart medicine for the rest of your life.
“If you go through EMS, you get that cath lab right away. You’re getting treated faster and may never have the need for rehab, bypass surgery, or maintenance drugs. This is saving money – and people – down the line.”
Flaws in the Payment Model
It’s not just the amount that EMS services are paid that’s a problem. There are flaws in the entire payment model for EMS, says Moore.
For example, ambulance services are only reimbursed for the actual rides (or transports) to the emergency room (ER). However, ambulance personnel are paid an hourly rate that is independent of the number of rides they provide. This means that if there’s a day where no transports are made, EMS won’t get reimbursed to pay the ambulance personnel.
“If you don’t do transports you don’t get paid. But we don’t just call people in whenever there’s a call. We have to have people sitting there because there is an expectation that an ambulance will be by your side within a few minutes.”
Then there’s the fact that all charges are bundled together. So, if an ambulance takes someone who is under cardiac arrest to the hospital, there is no separate charge for the stretcher, for the compressor or for the cardiac monitor.
“Nobody line-item charges anyone for an ambulance. You’ll see a rate and mileage charge. That’s it.”
Response Time Requirements Are Restraining
Many state and local government regulations set unrealistic response time requirements for EMS services to meet. Nationally, those requirements average at 8 minutes and 59 seconds. Although it seems like a good idea in theory, the requirements can have negative consequences, argues Moore.
“The truth is, 80 percent of calls are really not time-sensitive.”
For example, let’s say you have stomach pains for two days. While it’s likely that you can put up with another couple hours, you decide to call 9-1-1 instead of finding an alternative way to the hospital. According to Moore, under current contractual obligations to state and local governments, EMS must be at your door within 10 minutes. Moore considers this a huge issue that needs to change.
“We need to evolve the way we develop our response time requirements so we start saying ‘we will have someone to you shortly but they’re not going to be there within 8 minutes and 59 seconds. Based on the nature of what you told me, it sounds like it’s not acute.’”
Public Expectations Need to Change
Even if changes to protocols do occur, public expectations will continue to expect that a 9-1-1 call is followed by an ambulance at your door within minutes. Moore believes we need to better educate the public on why ambulances are so expensive in order to alter those expectations.
“The public’s expectation is that there will be someone at your door in less than 5 minutes and that is not the way it should be in many instances.”
The portrayal of emergency services in the media and on television reinforces this expectation even further, he says.
“We watch TV – where they get there and the patient survives. But most cardiac arrests do not survive; It’s just not the way it works.”
Minimize Your Costs: Inform Yourself
While Mr. Moore and the American Ambulance Association continues to advocate for changes in legislation to help reform the EMS system in the United States and to lower the price of ambulance rides, there are things you can do as a consumer.
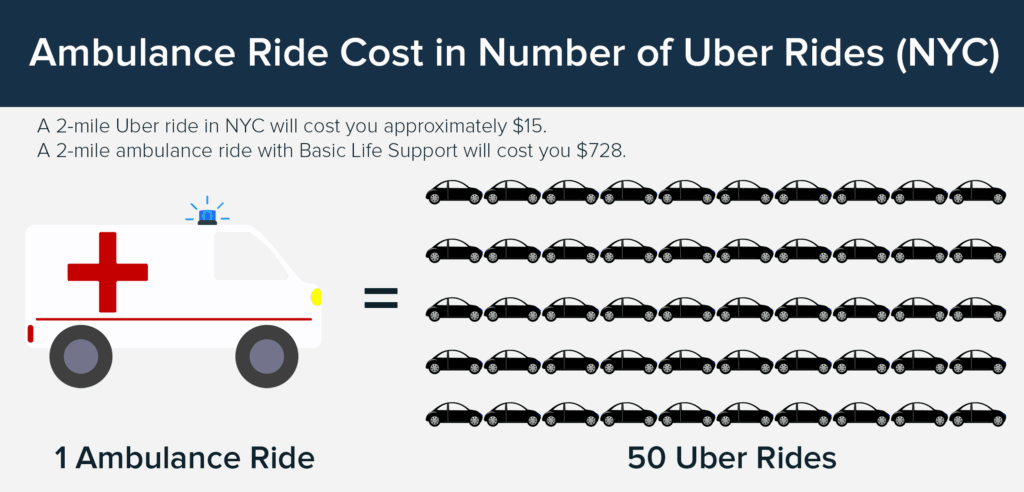
For one, you may be able to avoid to taking an ambulance to the ER in non-emergencies by using a taxi or ridesharing service to go to an urgent care center that, depending on the situation, may be able to provide you with the care you need.
However, it is always best to err on the side of caution. If you are unsure of the nature of the emergency, your safest bet is to dial 911 and hop in an ambulance.
“I’ve found that people who should’ve called 911, didn’t until it was too late. People who shouldn’t have called, call too often…The real message should be to get the right response, right care, at the right time, in the right place, in the most cost effective manner.”
You should also look into what your insurance policy covers for ambulance rides and which companies they contract with.
“People know what their co-pay is for their yearly physical but no one expects to call an ambulance so one knows what their policy is,” Moore says.
There are clear advantages to staying informed on these issues. For instance, if you’re at the hospital and need to be sent to a rehab center via an ambulance, it behooves you to know which ambulance company your insurance contracts with. This way, you can request that the hospital call the right ambulance company and save yourself the headache of covering your bill out-of-pocket.
According to Moore, our best hope for EMS is continued education.
“EMS is critically important. I’ve been on calls where had we not been there, the person would not be walking the planet. But there are a lot of dynamics that the public doesn’t realize and needs to learn more about.”
